Endometriosis Treatment in Chennai
The treatment for endometriosis varies depending on whether you are trying to conceive or not. If you’re not trying to conceive and your main problem is pelvic pain, while it’s more satisfying to have a ‘proven’ diagnosis, it is acceptable to treat the pain with medications (Depo-Lupron shots) without performing a laparoscopy first.
Birth control pills can help with the endometriosis symptoms and are often the ‘first-line’ hormonal treatment for endometriosis. Birth control pills contain estrogens and a progestin – progestin is an artificial form of progesterone which can reduce monthly growth of the uterine lining (endometrium) and can reduce growth of endometriosis implants which are outside the uterus, in your pelvis. Birth control pills reduce your ovaries’ estrogen production, and estrogen hormone is known to stimulate the growth of endometriosis. This treatment does not make endometriosis disappear, but is trying to make the disease less active, hopefully reducing pain.
Androgens (male-type hormones) also suppress endometriosis but may have bad side effects, such as deepening of the voice (rare) which does not get better if you stop treatment – so they are not used much anymore.
The ‘gold standard’ (best available) hormonal treatment is Depo-Lupron. This is an injectable medicine which can be given every month or every 3 months at our office. This puts you into a temporary, reversible menopause-like hormonal state where your body stops producing much estrogen from your ovaries – this takes away the hormonal stimulation of the endometriosis and can really make it ‘go quiet’ but not permanently go away. Side effects, include hot flashes, irregular bleeding and then no periods. Bone loss (osteoporosis) can be reduced by taking a daily progestin pill, with calcium and Vitamin D supplements to reduce bone loss and bone scans to monitor bone density if long-term treatment is needed. Some of our patients are pain-free for months or years on this treatment.
An alternative to Depo-Lupron is a pill called an aromatase inhibitor such as letrozole (Femara). This blocks estrogen production by your ovaries and the endometriosis tissue itself (which has the ability to ‘make its own estrogen’). This is a daily pill, and is easy to start and stop compared with Depo-Lupron. It can also be given along with a progestin.
In the near future we will have pills which have a similar effect to Depo-Lupron shots (oral GnRH antagonists) giving us another option …
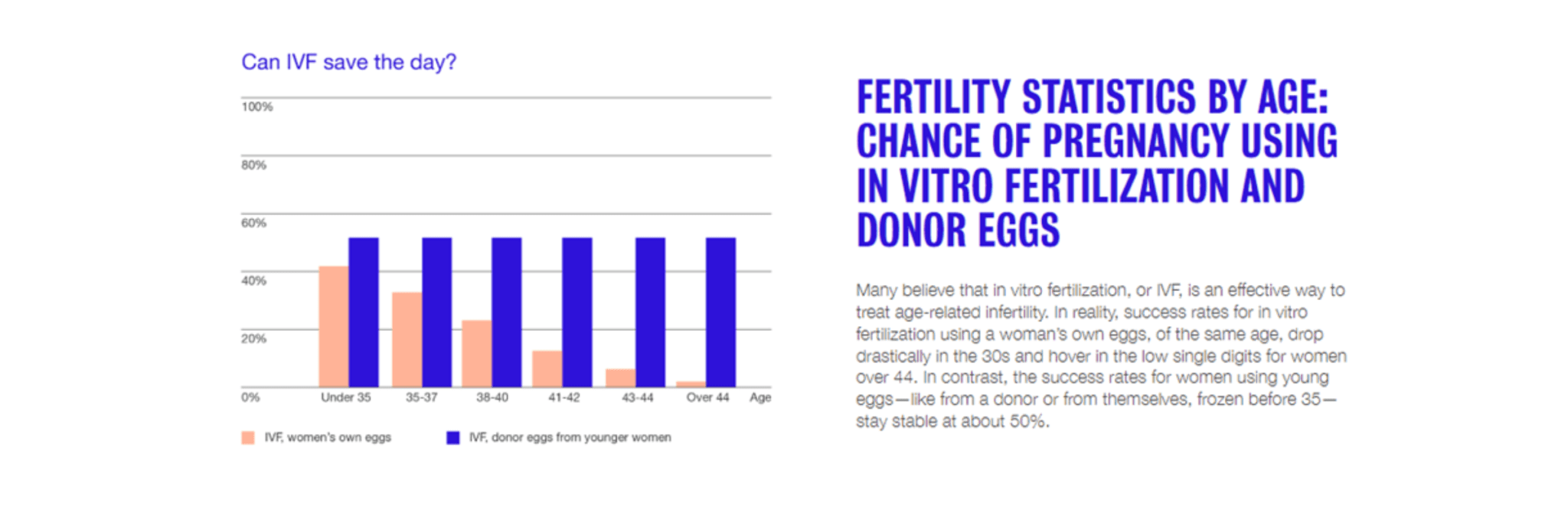
If you are trying to conceive, having endometriosis may change the course of your treatment in subtle or obvious ways. Having endometriosis (and surgical endometriosis treatment) may cause diminished ovarian reserve (low egg supply), scarring around the tubes or pelvic adhesions (scar tissue), or both. Some women with endometriosis need in vitro fertilization (IVF) to deal with these issues, and Depo-Lupron shots before IVF may improve success rates.
When is surgery required to treat endometriosis?
In general, you only need endometriosis surgery if you –
- Want to have kids and have a large endometrioma (endometriosis cyst within the ovary as well as severe pain)
- Are completely done with wanting kids and wish to have definitive surgery – removal of both ovaries (with or without hysterectomy).
Surgery rarely ‘cures’ endometriosis unless the surgery is removal of both ovaries (with or without hysterectomy). Removing both ovaries takes away most of a woman’s production of estrogen hormone which stimulates endometriosis tissue and causes it to grow.
Any other surgery (laparoscopy with laser treatment or cautery or excision of endometriosis, and/or removal of endometriosis cysts) may not remove all the endometriosis in your pelvis – even if your surgeon destroys or excises all visible spots of endometriosis on the surface of the uterus or behind the uterus, on or in the ovaries or on the pelvic side wall, there may be deeper areas of endometriosis not visible on laparoscopy which are missed. Endometriosis may also be hidden underneath areas of scarring.
Because of the above, some women get good pain relief after surgery to treat endometriosis, and some women don’t get good pain relief after surgery. Women with significant endometriosis (more than just a few spots on the surface of the uterus or ovaries) often do better with surgery to confirm the diagnosis and to treat visible disease, followed by Depo-Lupron injections to suppress any endometriosis that’s left behind, than with surgery alone. Surgery alone may provide short term relief of endometriosis pain (a few months up to a few years) before the disease and pain symptoms recur. Women who undergo multiple laparoscopies may get diminishing returns, with less and less pain relief with each successive laparoscopy.
Depo-Lupron can be used on its own without laparoscopy too – it also (but reversibly) takes away most of a woman’s production of estrogen hormone which stimulates endometriosis tissue. If you have pelvic pain symptoms suggesting endometriosis and your pain goes away with Depo-Lupron you are at least 80% likely to have endometriosis.
If you want to try to conceive and you have only small endometriomas, or early stage endometriosis without any endometriosis cysts visible on ultrasound, the surgery may do more harm than good by damaging some normal ovary tissue, which can reduce your ovarian reserve (the number of eggs left in your ovaries). Most people with endometriosis do not need surgery – it is only definitely needed for big endometriosis cysts or women who are done childbearing and have failed other treatment options. Unless you have both ovaries removed cure is unlikely, but you may get benefit in terms of reducing your pain for a period of time. Medical treatment with Depo-Lupron after surgery often gives better pain control than just surgery. Depo-Lupron can be used on its own without surgery, too.
What should I do if I think I might have Endometriosis?
Our board-certified physicians have extensive experience diagnosing and treating endometriosis. If you think you may have endometriosis, or have been experiencing any of the symptoms of endometriosis, you should contact us at PSFC to set up an appointment.
Your fertility with age
Egg is the quintessential part of a female reproductive system. You’re born with 1–2 million potential eggs (in the form of ovarian follicles). From this time, no new eggs are produced but that’s all the eggs you’ll ever have. Up to 1,000 eggs are lost each month. By puberty, your egg count might be half a million; at 25, maybe 300,000. Of these, only 300 to 400 will be ovulated during a woman’s reproductive lifetime.
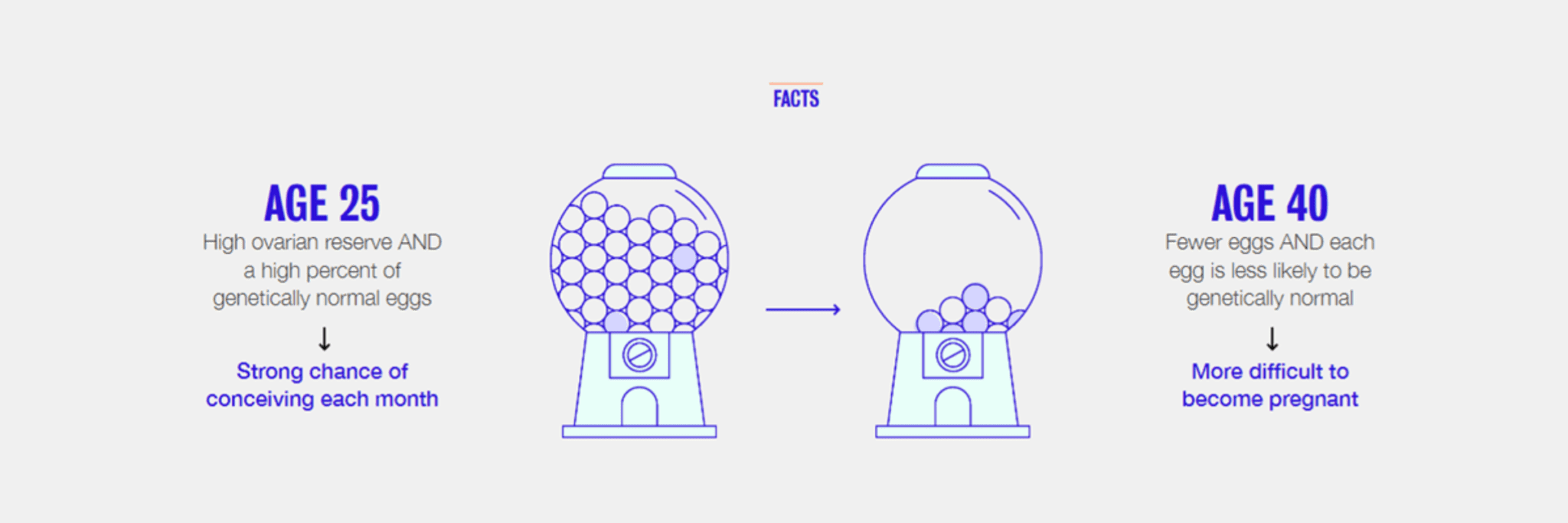
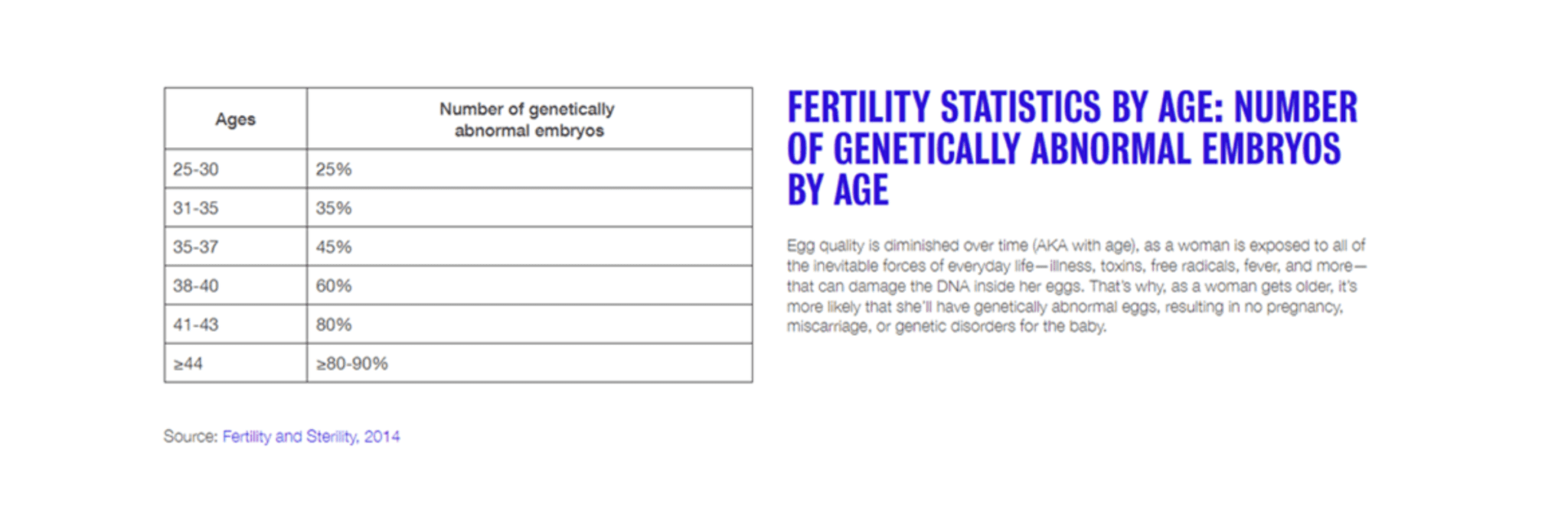
Fertility can drop as a woman ages due to decreasing number and quality of the remaining eggs.
Why does fertility decline so rapidly?
The two most common causes of female infertility are ovulation problems and blockages to the fallopian tubes as a result of infection. Ovulation problems can happen as you get older because:
Blockages to the fallopian tubes may be caused by infection or another condition. So, whatever your age, if you’re trying for a baby you need to take care of yourself. This means looking after your sexual health as well as your general health.
As a woman ages it is more likely that she may have had longer exposure to a condition that has not been treated. An untreated chlamydia infection, for example, can develop into pelvic inflammatory disease, blocking your fallopian tubes. This could prevent fertilisation altogether or increase the likelihood of an ectopic pregnancy.