Male Fertility Centre
Male infertility is a common problem, one that affects approximately 45% of couples having difficulties conceiving. It can be defined as any issue with the male’s biology that reduces the couple’s chances of conceiving. The good news is that with modern treatment techniques, even severe male factor patients can become fathers.
No matter the severity of the infertility in the men we treat, PSFC has the knowledge and tools to help them become fathers.
Symptoms of Male Infertility
Aside from being unable to conceive a child, other signs and symptoms of male infertility include:




Causes of Male Infertility

Varicocele

Infection

Hormonal imbalance

Difficulties with sexual intercourse

Sperm Blockage

Retrograde ejaculation.

Ejaculation Issues

Environmental Causes

Health & Lifestyle Changes
Diagnosis of Male Infertility
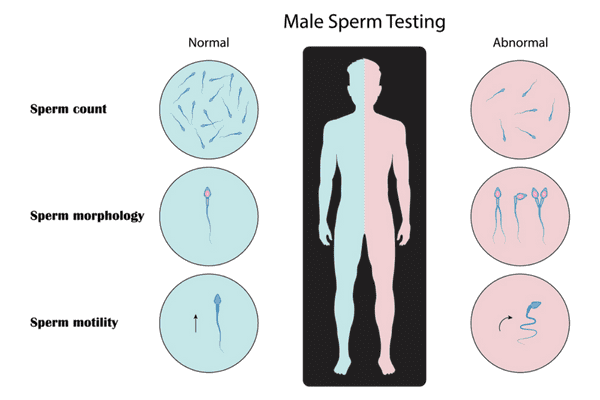
The initial diagnosis of male infertility is carried out primarily with a Semen Analysis. During a semen analysis we look at many different parameters, however, the three most important are:
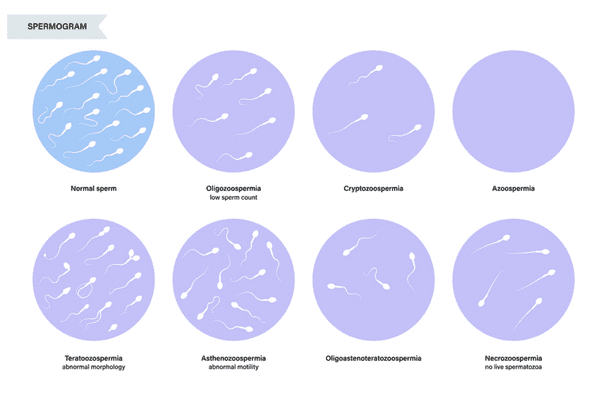
The above conditions can also be combined if a sperm sample exhibits multiple abnormalities. For example, a sample that exhibits all three conditions above will be labeled, Oligoasthenoteratozoospermic.
We also look at a variety of other less important characteristics that can effect how effective the sperm are such as: viscosity of the sample, forward progression of the sperm, and sperm agglutination (which can be an indicator that sperm antibodies are present).
Read More on Male Fertility FAQ’s
While a semen analysis is the primary test to diagnose male infertility, the truth is that each of the parameters above do not mean much by themselves. We fertility specialists look at is the big picture. Specifically, will the sperm be able to fertilize an egg? If the semen analysis comes back normal, it is very likely that sperm will function as it should. When one or more of the parameters come back abnormal then we can assume a problem may be evident based on the severity of the abnormality.
Other Semen Tests
In some cases, what we find in the original semen analysis can lead us to recommend additional testing.
1. Sperm Antibody Screening – There are two tests that assess for sperm antibodies. The first is a simple test called a MAR Screen. The MAR screen is a test that rules out sperm antibodies, however it cannot confirm the presence of sperm antibodies. If the MAR comes back positive, then a more accurate Immunobead Test (IBT) will be ordered to conclusively confirm the presence of the antibodies. For reference, the presence of sperm antibodies can interfere the ability of sperm to fertilize an egg.
2. Sperm Viability Testing – This test is for sperm samples that exhibit a very low motility and is used to assess what percentage of the sperm are alive. It is possible for sperm to still be alive and able to fertilize an egg, and exhibit zero motility.
3. Leucoscreen – This test is ordered for semen samples that contain a high round cell count. Round cells are commonly found in the ejaculate and can be a variety of different cells. A luecoscreen is ordered to determine if any of the round cells are white blood cells (leukocytes). The presence of white blood cells can be an indication of an infection, which should be treated as soon as possible after the initial diagnosis.
Treatment for Male Infertility
Treatment varies depending on the cause, and severity of the male infertility. In mild cases use of IUI (Intra-Uterine Insemination) itself may be sufficient. During an IUI the semen sample is concentrated and cleaned in the laboratory and then injected directly into the uterus. If the cause is hormonal in origin then hormone treatments might be recommended. Some mild cases can also be treated through lifestyle changes. However, it is important to note that any lifestyle or medical intervention that a man goes through in order to improve their sperm count will take time to be effective. The male sperm production process is a lengthy one that takes about three months from start to finish. This means that it can take up to three months for any changes to make a noticeable difference.
In more severe cases, IVF with or without ICSI may be indicated. Through the use of ICSI, we can achieve very high fertilization rates, even in severe male factor cases.
Even the most severe cases of male factor infertility, where there is no sperm in the ejaculate (clinically referred to as azoospermia) can be treated. If you have been diagnosed with azoospermia there is still a possibility that you have some degree of sperm production in the testes, but its delivery to the ejaculatory ducts has been blocked. In these cases, surgery can be used to determine if there is still sperm being produced in the testes, and if so to retrieve enough for fertility treatments. The most common type of surgical intervention is a testicular biopsy (sometimes called a testicular aspiration). This procedure can be used to further diagnose the issue and retrieve enough healthy sperm, if they are present, to be used in an IVF cycle paired with ICSI. It is also possible to freeze the sperm for use in a later IVF cycle, or to use one aspiration for multiple cases if enough sperm are found. However, this will vary depending on individual factors. We almost always recommend a fresh sample whenever possible as the freezing/thawing process is detrimental to sperm quality and, generally, only a small amount of sperm is obtained through these procedures.
Whatever the cause, our specialists at ORH have extensive training and experience with the diagnosis and treatment of male infertility. Please contact us if you have any questions or would like to schedule a consultation to discuss your options.
Although many of the specific causes of severe male infertility remain unknown, it is estimated that almost 50% of cases may be due to contributing genetic factors, and there are over 30 known genetic diseases that will cause infertility in men.
Throughout history, men afflicted by such diseases were faced with the tragic realization that they would never father children of their own, yet their infertility also created a barrier to the hereditary transmission of such illnesses. With the advent of ICSI, most of these men are now capable of fathering children – and many are choosing to do so. The main concern of these men is the chance of passing their condition to their offspring. Technologies such as pre-implantation genetic screening (PGD) allow the selection of embryos that do not carry the problematic gene. However, the technology is limited, as its application depends on the nature of the particular genetic condition. For conditions caused by a single dominant gene, it is relatively easy to screen and eliminate the embryos with the malfunctioning gene. For conditions caused by a pair of recessive genes – such as in the case of cystic fibrosis – affected fathers will inevitably pass one of the genes to their child. Said child must be vigilant as to whether their partners may be carriers as well when they seek to have children of their own.
Furthermore, there are many heritable genetic defects that do not carry the same severe consequences to overall health yet will cause severe refractory infertility. One of the most common, a microdeletion in the azoospermia factor (AZF) region – specifically region AZFc– causes severe infertility , yet TESE may yield enough sperm to pursue ICSI. Many men diagnosed with AZFc choose to have children through ICSI, and unavoidably pass on the mutation to their offspring, thus too becoming infertile. AZF deletions are relatively common in cases of severe male infertility, and thus clinics will often screen severely infertile patients for the genetic defect. Those found to have the defect are presented the choice of continuing with ICSI with full knowledge of the consequences, yet one study found that almost four-fifths of prospective parents decided to pursue ICSI regardless.
The moral consequences of such decisions cannot be taken lightly. Men with diseases such as cystic fibrosis (or other deadly genetic illnesses) who choose to have children must also consider the impact of their likely early death on their prospective children, as most of these men do not live to see past 40. Children with inherited AZFc microdeletions will experience their infertility as an established fact, and parents of such children will face hard decisions on how and when to tell them. Furthermore, the cumulative societal effect of conceiving infertile children through ICSI may become problematic. A study in the reputable journal Nature Genetics estimated that, if 90% of men that are infertile due to genetic causes fathered children through ICSI, the rate of male infertility due to a genetic basis could increase to 6.7% of all men in 10 generations. Due to barriers in accessibility and cost, this dire situation is unlikely, yet still illuminates a probable trend as assisted-reproduction technologies such as ICSI become more ubiquitous in society.

