Many people tend to think of fertility as something that pertains primarily to women, but in actuality, at least 30% of infertility cases can be attributed to male-factor infertility. This guide to male fertility testing will explain what the options are, when—and why—a man should test his fertility, and what happens if you don’t get the result you’re hoping for.
The Cornerstone Of Male Fertility Testing: The Semen Analysis
The first step in male fertility testing is the semen analysis. A semen analysis is a fairly simple, non-invasive test in which a semen sample, typically produced via masturbation, is examined under a high-powered microscope to determine the quantity and quality of sperm.
What A Semen Analysis Tests For:
Sperm concentration (quantity)
Sperm concentration is the measure of how many sperm are present per milliliter of semen. Sperm concentration is found by calculating the number of sperm per milliliter of semen. A normal sperm concentration, according to the World Health Organization, is at least 15 million sperm per mL.
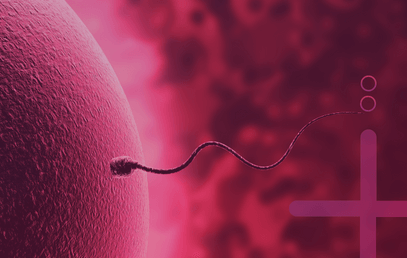
Why is sperm concentration important for male fertility? Because, after ejaculation, the sperm encounter many obstacles on their way to the egg: the acidity of the vagina, the cervical mucus (which can either help or hinder sperm’s journey toward the egg), and the possibility that they could get stuck somewhere else in the reproductive system—like up the wrong fallopian tube. Experts estimate that less than 1% of sperm actually make it to the egg, so it makes sense that it’s helpful to start with a lot.
Sperm motility (movement)
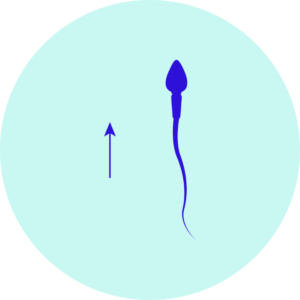
Sperm motility refers to how sperm move. Sperm are propelled forward by flagellations of their tail, plus a little help from the female reproductive system. The movement of sperm impacts whether or not they make it to the egg, and—once they do make it—whether they can penetrate the egg to fertilize it.
The ideal way for sperm to move is in straight lines or in large, sweeping circles. Motility is a measure of what percentage of sperm are moving, and progressive motility is a measure of what percentage of sperm are moving in this optimal way. According to the WHO, at least 40% motile sperm (with at least 32% moving progressively) is a normal result.
Fun fact: While it was believed for centuries that sperm moved forward thanks to quick back-and-forth movements of their tail (kind of like fish), a groundbreaking study published in July 2020 revealed that sperm actually “roll as they swim, much like playful otters corkscrewing through water.” This doesn’t change the importance, or the measurement, of motility, as the corkscrew motion can only be seen with super high-tech equipment—but it does give sperm a little more personality.
Sperm morphology (shape, size, and structure)
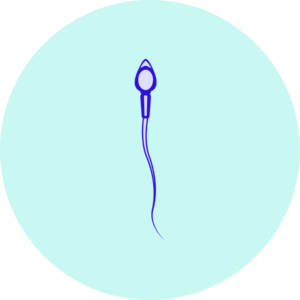
The proper sperm anatomy, according to male fertility company Legacy, looks like the following:
- a tail, which helps it “swim” toward the egg,
- a midpiece, containing mitochondria to power the sperm’s movement,
- a head, housing the nucleus (where genetic material for the potential offspring is stored), and
- an acrosomal vesicle, a structure at the tip of the sperm that contains enzymes to help the sperm penetrate the egg.
If a sperm is deformed—if it has multiple heads or tails, no head or tail, improperly formed sections, or it’s too big or too small—it may have difficulty moving toward the egg or fertilizing it. Morphology is the measure of what percentage of sperm have the proper shape, size, and structure, also known as “normal forms” (NF). According to the WHO, a normal morphology result is 4% NF or higher.
Semen factors
Semen volume refers to the amount of fluid that’s ejaculated. Typically, a low semen volume—less than 1.5mL according to the WHO—alone is not going to greatly impact male fertility, but it can indicate a blockage in one or more of the ducts/gland of the male reproductive system, and can compound the issue of low sperm count.
In addition to volume, male fertility testing may evaluate the pH level and chemistry of the semen. Again, abnormalities in semen pH or composition may point to a problem in the testicles, such as an obstruction or infection.
All four of the above “semen parameters” are important to consider when talking about male fertility testing.
In-office Vs. At-home Male Fertility Testing
A semen analysis is often performed in a fertility or urology office where there’s an andrology (male health-focused) laboratory. The process goes something like this: the male patient receives a sterile specimen cup for his semen sample. He can collect the sample, via masturbation, either in a “collection room” at the office, or produce it at home and bring it to the office, ideally within one hour.
The experience of producing or providing a semen sample at the office, while very common and nothing to be ashamed of, can be uncomfortable for many men. That’s why companies like Legacy offer at-home sperm testing kits that allow patients to collect their sample in the comfort of their own homes, combine the sample with special preservation media, and then mail it to the lab. This eliminates the need to go into the office at all, making it more convenient and less awkward.
A note of caution: many at-home male fertility testing products only test for sperm count, which—as we discussed above—is only part of the picture of male fertility. Make sure that, if you go this route for male fertility testing, the product you choose offers a comprehensive report on all sperm parameters.